Towards a UN Security Council on Global Health Issues – EU Institutions Could Show the Way through Adapted HERA
In the April/May 2021 article by Sergio Aguirre and William Wagner for the journal Survival [“What’s the UN Council For?”, Survival vol 63 n.2, April-May 2021] of the London based International Institute for Strategic Studies, the authors argue how the 75-years-old United Nations’ Security Council (UNSC) has to renew itself to face new threats in order to remain a relevant international body to help protect future generations. Among these global menaces, Mr Aguirre and Mr Wagner highlight how global health is deeply interconnected to international peace and security, “and therefore within the [Security Council]’s remit”. Even though the five permanent members of the UNSC tend to block discussions on emerging transnational threats pertaining to themselves to not appear vulnerable in the eyes of possible opponents, the authors argue that the Security Council is now ready to take on the challenges of global health, as two historical precedents demonstrate. The first one refers to the Security Council’s response to the Ebola virus in West Africa in 2014. With its Resolution 2177, the UNSC declared Ebola a threat to international security and peace, thus inciting the UN to accelerate its response to the virus with the creation of a special system-wide coordination and organizing the UNSC as a forum to deliver assistance. The second and most recent precedent regards the handling of the COVID-19 pandemic. In this case, the UN Secretary General pleaded for a worldwide ceasefire to focus on the response to the pandemic, which was briefly respected in the case of the war in Yemen.

Already in June 2020, the PA International Foundation presented a very similar proposal to the Independent Panel on Evidence Against Antimicrobial Resistance (AMR), a body established in line with the recommendations of the UN Interagency Coordination Group on Antimicrobial Resistance (UN IACG) that at the time was inquiring what actions the UN should take to best prevent AMR. The Foundation argues that – like preventing wars by preparing for them (‘si vis pacem, para bellum’) – pandemics require optimized measures of preparedness to prevent them. Such preparedness has successfully been realized through the North Atlantic Treaty Organisation (NATO) and its Allied command structure and ‘forward defence’ strategy. In a document presented to the European institutions and global health experts the Foundation pleaded to expand the European Commission’s current European Health Emergency Preparedness and Response Authority (HERA) with an agency similar to the European Defence Agency (EDA) that is led by EU Member States – and thus bridges the lack of harmonized EU health policies. It is indeed EDA that gains in prominence following a clearly sensed urgency for the EU Member States to strengthen their grip on foreign and security policy in a post-Trump era with worsening perceptions of Chinese and Russian foreign and security policies. While HERA is considered a positive development, bridging interinstitutional infighting to better defend European citizens’ (health and security) interests through a European Health Security Council as part of HERA at Heads of Government level may well offer the most immediate success (please refer to the links one and two for the full text of the PA International Foundation proposal).
This is all the more urgent following the address by European Health Commissioner Stella Kyriakides during a Global Health Conference organized by the past Portuguese Presidency of the Council (26 March 2021). She referred to antimicrobial resistance as the next pandemic to be prevented. In their letters to the Foundation of 22 July 2021 and 7 June 2021 both Commission President Ursula von der Leyen and Health Commissioner Stella Kyriakides thanked the Foundation formally for its global conferences and website on AMR.
At EU level, PA’s work has been particularly focused on spreading awareness through www.stopAMR.eu and by identifying solutions to the antibiotic market failure dimension of AMR. But the imminent danger is larger than that. In the proposal to the Independent Panel on Evidence Against Antimicrobial Resistance, PA suggested that AMR must be part of UN Security Council deliberations as AMR threatens to kill more people than any war so far has managed to kill. The post-antibiotic era announced by then WHO Director General Margareth Chan may hit within just a few years; over the past 20 years the European Union already mourns 400,000 AMR deaths. This may grow to 10 million people per year globally by 2050. In this sense, the UN Security Council has to become involved to secure broadly supported and timely effective action to prevent AMR; otherwise, a future AMR outbreak will have a far more ruinous effect on the world’s population and economy than COVID-19. The Security Council also seems the only platform that can address the industrial reality behind the rapidly growing AMR crisis: continued overproduction and overuse of antibiotics over decades without developing any new categories of antibiotics. This was already established during the UN Special Session on AMR of 21 September 2016 which led to the creation of the UN IACG. Overseeing practical results since requires humanity to secure that the UN Security Council – after Ebola – puts pandemics and notably AMR on its agenda. In so doing a measure of global consultation and cooperation may be added to the current rather negative trends.
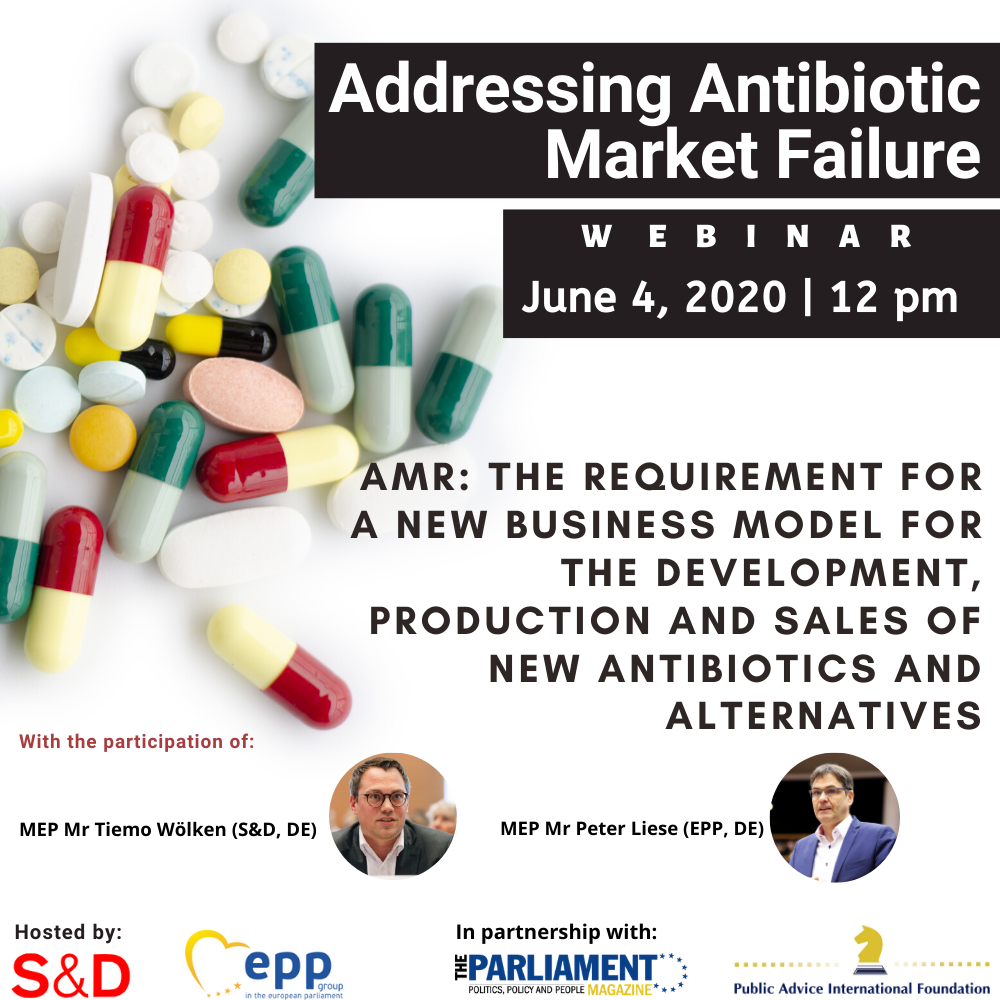
According to a Euractiv article from 23 July 2021, EU institutions are now being urged to consider the full range of new incentive systems and pilot innovative approaches to tackle antimicrobial resistance (AMR). While the development of new antibiotics is seen as a solution to cope with this ‘silent pandemic’, their availability in many countries across the EU has proved to be particularly difficult as some of them are not commercially launched, even despite being approved by the authorities (EMA). According to Remko van Leeuwen, CEO of the biotech company Madam Therapeutics and board member of the BEAM (Biotech companies in Europe combating antimicrobial resistance) Alliance, the cost of bringing and keeping antimicrobials to the market is too high to offer an incentive for a private company to invest. The PA International Foundation in 2020 already hosted BEAM during a high-level Webinar but ever since the problem is not resolved. The Euractiv article reports that in 2020, the global pharmaceutical industry invested nearly 1 billion US dollars in the AMR Action Fund to develop between two and four new antibiotics to patent by 2030. However, as executive director at CARB-X and professor of law Kevin Outterson explains, there are drugs approved by the European Medicine Agency (EMA) that are not yet launched in EU countries because the additional cost of launching is not worth it, compared to the reimbursement they receive.
Policy manager at European Public Health Alliance (EPHA) Yannis Natsis affirms that, since the launch of the One Health approach in 2017, the EU does promote meaningful innovation in the fight and prevention of antimicrobial resistance. Now new incentive systems and approaches are proposed to the EU lawmakers to effectively tackle AMR. While it is good that the Commission has evolved from studying the AMR issue to taking action, an AMR outbreak may come sooner than effective action to prevent it. In Great Britain, a ‘Netflix-style’ subscription service, regularly paid from governments to the pharmaceutical industry, has been recently proposed and experimented to incentivise the creation of new antibiotics. According to the article, European ‘pull’ incentives are seen by some as the best instrument to reassure investors, as they pay for results rather than for the effort on the part of researchers, creating incentives for private sector engagement by creating viable market demand. However, in this regard the European Commission is considering whether to pilot innovative approaches to research and development (R&D) and public procurement for antimicrobials and their alternatives.“We put additional funds into the R&D budget of the European Union, but still we don’t see results,” said Andrzej Rys, director for medical products and innovation at the Commission’s DG Sante, adding that this difficulty led the EU executive to mull over the pull model.
A new approach that would create a viable proxy market while creating minimal profitability for producers may be the best solution to correct the current market failure in the sector. “Pharmaceutical companies have dropped the ball on AMR for decades now. No new class of antibiotics has been discovered in over 30 years using the usual market-based business model of the pharmaceutical industry,” affirmed EPHA’s Yannis Natsis to Euractiv. The world spends billions of USD on the funding of multinational enterprises to develop new medicines but – quite apart from the market failure – mostly Small and Medium Sized Enterprises (SMEs) are the ones developing new antibiotics. And because of the market failure these SMEs cannot survive.

Therefore, the PA International Foundation proposes that a proxy trade model should be engineered: with national EU strategic reserves becoming buyers and UN Member States becoming funders and off-takers through a Global Fund specifically designed for tackling AMR. A first and successful debate on this matter by the UN Security Council could set this in motion. On top of this, the model provides no rewards in case of lack of industrial success: if a company fails to produce the new antibiotic it agreed to develop, it will be responsible for this failure and will not be compensated by taxpayers for a drug that failed to reach the market. A key mechanism enshrined in this proposal is the complete uncoupling of profit from sales volumes. Under this model Member States reserve drugs from a company and use these only when necessary (last resort). Drugs not needed for an individual Member State’s healthcare system are instead kept in strategic reserves for use when needed internally or externally – and in so doing the preparedness and prevention takes shape. The stockpile of these critical new antibiotics can, when required, be exported to third-party countries experiencing an outbreak of resistant bacteria and paid for through a Global Fund for AMR. This is done in very well-understood self-interest of ‘the West’; COVID-19 and particularly the Delta variant teach us all that not helping developing countries backfires on those that could have helped but did not. And so the UN Security Council dimension will secure that this ‘forward defence’ does not only defend the richer part of the world, but, from scratch, ALL.
In the past year the World Health Organisation – according to some already heavily politicised – has been subjected to severe criticism. Matters seem improving, but the learning process may be too slow for comfort. Only the UN Security Council may be able to map a faster and better way forward as in the Ebola case. The European Union, through the initiatives of both the European Council and the European Commission, could demonstrate unity of purpose by a joint call on the UN Security Council to move in the required direction.


 Report
Report


